“Of pain you could wish only one thing: that it should stop. Nothing in the world was so bad as physical pain. In the face of pain there are no heroes.” – George Orwelll
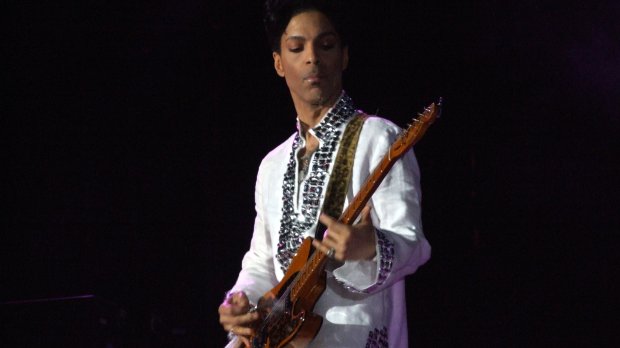
It has now been a year since the iconic singer, songwriter and performer, Prince aka Prince Rogers Nelson, was pronounced dead. One week after a mysterious emergency plane landing and hospital visit, Prince was found unresponsive in the elevator of his Paisley Park home in suburban Minneapolis. Medical efforts to revive him were unsuccessful.
And over the last year, while the fifty-seven year old musical sensation was mourned and eulogized in tribute after tribute, the sad reality remains: Prince didn’t have to die. Investigators have revealed that Prince overdosed on a potent narcotic known as Fentanyl. Medications found surreptitiously tucked away in numerous bottles labeled as aspirin and Vitamin C were a stashed supply of Hydrocodone/Acetaminophen (also known by the brand name, Vicodin or Norco). But on further analysis, the presumed Hydrocodone/Acetaminophen were, in fact, counterfeit pills comprised of the potent narcotic Fentanyl, Lidocaine and other components. What was likely Prince’s attempt to self-medicate and assuage an addiction with illicitly-obtained pain medications resulted in a deadly and inadvertent overdose.
This tragedy reminded me, once again, of the vexing problem of pain.
As an internal medicine physician, pain is something I see all the time. Day after day, I encounter an aging adult population with maladies as diverse as osteoarthritis to sciatica, migraines to metastatic cancer, motor vehicle accidents to post-surgical pain. Pain is one of the most common reasons for visits to the doctor’s office, and as a practitioner charged with healing, I want to do my best to help.
But there are problems with pain.
- Pain is subjective. We have no lab, no imaging test, no failsafe question that can effectively capture pain in a truly objective fashion. As Graham Greene once wrote, “This pain of mine is individual, this nerve that winces belongs to me and to no other.” Oh yes, we have inflammatory markers that can soar and imaging studies that can show bad bone breaks or aggressive invasive cancers, but even these are surrogates for what the patient actually feels. One person with back pain has a completely normal MRI. Another with no complaints has an MRI that makes a battle-tested neurosurgeon blanch. Different maladies engender different pain in different people (and even in the same people at different times). This doesn’t mean that pain is not real – just ask any birthing mother or patient passing a kidney stone to deny its reality. It just means that our capacity to objectively qualify or quantify it is woefully inadequate.
- Sometimes people are dishonest about their pain. Sometimes. This is more the exception than the rule, but it complicates a physician’s safe and effective approach to pain management. Addiction with encroaching symptoms of withdrawal can lead to drug seeking. Patients can have secondary gain by dishonestly seeking workman’s compensation, disability payments or success in a lawsuit related to an accident.
- Sometimes the source of pain is incurable. It is always rewarding to see improvement in patients after they receive definitive interventions for appendicitis, kidney stones, acute coronary syndromes (aka heart attacks) and biliary colic (obstructing gallstones). But what about patients on maximal medical therapy for rheumatoid arthritis, severe osteoarthritis, migraines and metastatic cancer? And how about the more elusive chronic pain syndromes such as chronic prostatitis, fibromyalgia, or chronic pelvic pain?
- Pain medications have their own problems. While pain medications can offer relief and even alter the natural history of some maladies, they must be used with care. Excess Tylenol use can adversely impact the liver. Too many NSAIDs (Non-Steroidal Anti-Inflammatory Drugs like ibuprofen, naproxen, Celebrex, etc.) can impact kidney function, risk peptic ulcers and even heart attacks. Nerve pain medications (Neurontin, Lyrica, etc.) can cause unsteadiness, confusion and weakness. And narcotics (Vicodin, Percocet, Morphine, Dilaudid, etc.) can constipate, cause confusion and falls, and risk addiction. And on top of all of this, the medications may simply not help. While all of these medications can be used safely and successfully for legitimate reasons, their problems require them to be prescribed and used judiciously.
So what does one do?
- Physicians should give people the benefit of the doubt. The subjectivity of pain doesn’t discount the reality of it. Listen to their story, offer empathy and think critically about how to address the root of the pain and to judiciously alleviate that which remains.
- Remember the options for pain control beyond medication. Physical therapy, steroid injections, exercise and weight management, biofeedback, surgery (if indicated), cognitive therapy and even patience are all options/adjuncts that may help with pain management.
- If a pain medication is necessary, when able, always choose the least problematic medication that will manage the pain. Many people are surprised when Extra Strength Tylenol or ibuprofen on a short term scheduled basis (under a doctor’s guidance) can do for them. And, many people are unaware of the potential adverse effects of many stronger pain medications.
- If pain is intractable in spite of reasonable medications/interventions, refer to the appropriate specialist (neurology for migraines, rheumatology for arthritis, etc.), including pain specialists so that the root cause or the tenacious symptoms are managed in a safe, yet optimal way.
As we look back upon the year that has passed since Prince’s death, we are again reminded that he didn’t have to die. The trial of a painful condition led to narcotic overuse, overuse led to addiction, addiction let to surreptitious use, and that surreptitious use led to death by an unregulated (likely unintentional), deadly ingestion of Fentanyl. It didn’t have to happen. And physicians and patients can learn from this.
Let there be no doubt, the problem of pain will always be with us. And as C.S. Lewis wisely reminded, “Pain insists on being attended to.” So let us endeavor to attend to the problem of pain thoughtfully, conscientiously and safely.
There is no better way.